Above & Beyond Billing
Optimize Your revenue with a full-fledged financial system
Revenue cycle management is the process of managing all the activities that occur in the billing and payment cycle for a hospital, health care organization, or physician practice. This includes tasks such as claims processing, billing, collections, accounts receivable management, insurance eligibility verification, and medical records coding. While it’s called “revenue cycle management,” the process doesn’t just focus on revenue generation.
You’ll also see references to “patient financial engagement” which is about communicating with patients and gaining their trust. For many health care providers, a large part of revenue cycle management is about getting payment from an insurance company for the services provided by a hospital or physician practice.
A hospital’s revenue cycle department is usually organized into three main areas: the billing department, accounts receivable, and contracts. For a physician’s practice, you’ll often see revenue cycle management focus on medical coding and billing.
The Revenue Cycle Management Department at a Hospital
Optimize Your revenue with a full-fledged financial system
Hospitals have a dedicated revenue cycle management department with a chief financial officer to oversee the main functions of the department. These include: Billing/collections – This involves collecting payment from patients or insurance companies for the services and procedures provided at a hospital or ambulatory care center.
.This involves collecting payment from patients or insurance companies for the services and procedures provided at a hospital or ambulatory care center.
Accounts receivable – This area of revenue cycle management focuses on accounts receivables, which is the total amount owed to the hospital by patients.
This area of revenue cycle management focuses on accounts receivables, which is the total amount owed to the hospital by patients.
Financial solutions – This area of revenue cycle management includes payment plans and financial assistance for patients who can’t afford to pay their entire hospital bill.
This area of revenue cycle management includes payment plans and financial assistance for patients who can’t afford to pay their entire hospital bill.
Coding and clinical documentation improvement – This area of revenue cycle management is about providing financial, coding, and billing software that complies with the latest industry standards.
This area of revenue cycle management focuses on analyzing and maintaining records for individual patient accounts.
Compliance – This area of revenue cycle management involves complying with all federal, state, and local regulations that apply to healthcare claims and billing processes.
HealthQuest RCM is the answer
HealthQuest RCM‘s Revenue Cycle Management solutions provide you with the tools to optimize your billing and account receivable processes, automate revenue workflow, and reduce regulatory compliance risk. Using HealthQuest’s market-leading clinical RCM solutions, you’ll get the most intelligent automation software available today, complete with advanced analytics and visual options. You’ll be able to improve your bottom line while complying with PAMA and FASB reporting requirements.
Make An Appointment
Have any Question?
Book an appointment
Have care Requirement?
Call the hospital
Why Choose HealthQuest RCM?
Introducing HealthQuest RCM, the leading provider of Revenue Cycle Management (RCM) solutions. Our advanced AI-automatic software is designed to help you achieve peak financial performance, no matter what size your business may be. With our expert team of billing specialists and RCS visibility, business intelligence, and analytics diagnostics providers, you can confidently manage your revenue cycle for maximum efficiency.
How HealthQuest RCM Deliverance Value?
Certified Coders & Molecular Lab Billing Expertise
Business Intelligence for Reporting
Success and Managed Services
Strong Workflow Automation
Expertise and Managed Services
Financial Integrity & Development
When I look at Healthquest I look at them as Operators, we don’t look at them as consultants. There was always a conversation about why did we outsource. Unfortunately, we have to change several software and applications in past but selecting the right revenue cycle partner is like security assured income.”
Group Practice
“We are glad to meet partners, not a third-party vendor who knows out-of-network billing with top insurances. Healthquest creates a better environment for the sales reps and we will be able to grow our volume and revenue and achieve a better outcome.”
Our Client
We never had an idea to validate genetic services in our chain of labs special thanks for HealthquestRCM Validation-Molecular and Revenue Cycle team we are delighted with your services and knowledge
Lab Manger
WE HAVE BEEN SERVING OUR CLIENTS IN THE FOLLOWING STATES
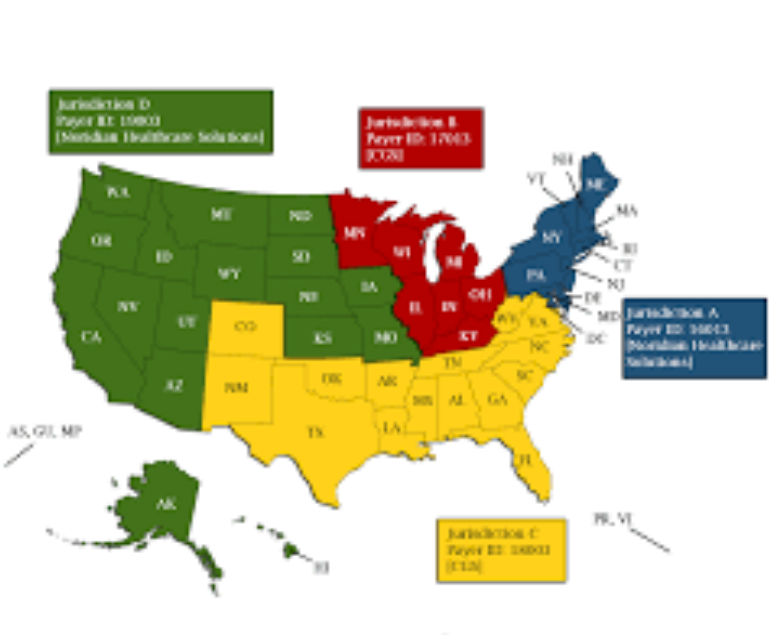
- Arizona

- California

- Colorado

- Delaware

- Alabama

- South Carolina

- Florida

- Georgia

- illinois

- Indiana

- Kansas

- Kentucky

- Maryland

- Michigan

- Mississippi

- Missouri

- New Jersey

- NewYork

- NorthCarolina

- Ohio

- Oklahoma

- Pennsylvania

- Tennessee

- Texas

- Vermont

- Virginia

- Washington

