Did you know that the sheer volume of the work and the complexity involved cause the job rate of provider enrollment and credentialing services to increase daily in the USA? You’ll be surprised to learn that half of the group still doesn’t understand the fundamentals of the job, though.
Besides, one of the most frequent queries from newcomers is what the distinction between provider enrollment and provider credentialing is. So, If you fall into this category, this article will guide you through the specifics of the process and outline everything you need to know about the various systems.
Still, before you begin working, you should be aware of the following differences between provider credentialing and enrollment:
What does provider enrollment mean?
- In the USA, numerous insurance companies, both large and small, offer a variety of health insurance plans.
- A health plan is offered by one or more of these insurance providers to an insured person.
- When a patient needs medical services, they typically look up the health plan’s network of hospitals or other providers.
- To be paid for the medical services they provide, a provider must be “enrolled” in one or more of these health plans.
What do we mean by provider credentialing?
- To enroll in any health plan, the provider must submit an application to the relevant insurance network.
- The provider credentialing procedure is the first step of the application.
- The insurance staff records all of your information during this phase, including your demographic information and the most recent professional training you have received.
- The gathered data is then approved after going through a preliminary verification process.
What are the procedures for enrolling a provider?
- The procedures for enrolling a provider can differ between different payer networks. The steps are frequently hazy and challenging to comprehend.
- However, after the documentation has been gathered, the first step is to credential the concerned provider.
- After the credentialing procedure is complete, the provider should anticipate additional inquiries about their educational background or any prior employment, depending on the payer network vacancy.
- The provider enrollment specialist assists the provider in completing these crucial first steps.
What procedures are involved in provider credentialing?
The purpose of provider credentialing is to assess the expertise of the medical professional and confirm the validity of all supporting documentation. As a general rule, the following fundamental steps are taken:
- The payer network requests a number of documents pertaining to the provider’s information.
- However, each payer may have different requirements for supporting documentation.
- Name, address, contact information, academic credentials, credentials for medical residency, and credentials for training are all considered standard information.
- The requirement for board certification in the case of specialization
- Sometimes the role may also need to be supported by any research the provider may have conducted while they were in training.
- The credentialing committee subsequently sends this information to primary sources for confirmation.
- The provider might also be required to provide some additional documents if there is any discrepancy.
What duties do provider enrollment specialists perform?
- On behalf of the healthcare provider, the provider enrollment records information from the various health plan applications.
- The specialist creates priority lists regarding which application needs your attention right now because the application is a lengthy process with multiple deadlines.
- For the process to go smoothly, it is best to make sure that you turn in all required paperwork and any additional responses well before the deadline. That is handled by the enrollment specialist as well.
- The expert can advise the provider on the types of plans that take effect retroactively in the case of government payer plans like Medicare and Medicaid. Moreover, the provider’s cash flow may benefit from these programs.
- In addition to all generic work, the specialist handles any additional tasks needed by the provider to complete the final step of payer network enrollment.
What exactly falls under a provider credentialing specialist’s purview?
- A credentialing specialist concentrates on collecting the provider data needed by the payer network and verifying it.
- The provider gives the credentialing specialist all the data that is listed in the credentialing packet.
- To find any gaps in the data or inconsistencies, the specialist runs all of the data through the primary source verification process.
- Even though it takes a while, the procedure is organized and simpler than enrollment, which occasionally lacks clear requirements.
How lengthy are the procedures?
- Enrollment and provider credentialing both take a long time. It can last anywhere from a few days to a full year.
- The credentialing process typically takes between 90 and 120 days to complete.
- If all the necessary information is provided or the provider has an existing contract with the payer network, the remaining steps in the enrollment process after credentialing are expedited.
- The enrollment process may be unnecessarily delayed if the provider takes too long to submit the information and supporting documents.
- It is therefore advised to have all of your documents organized before applying to the various insurance networks.
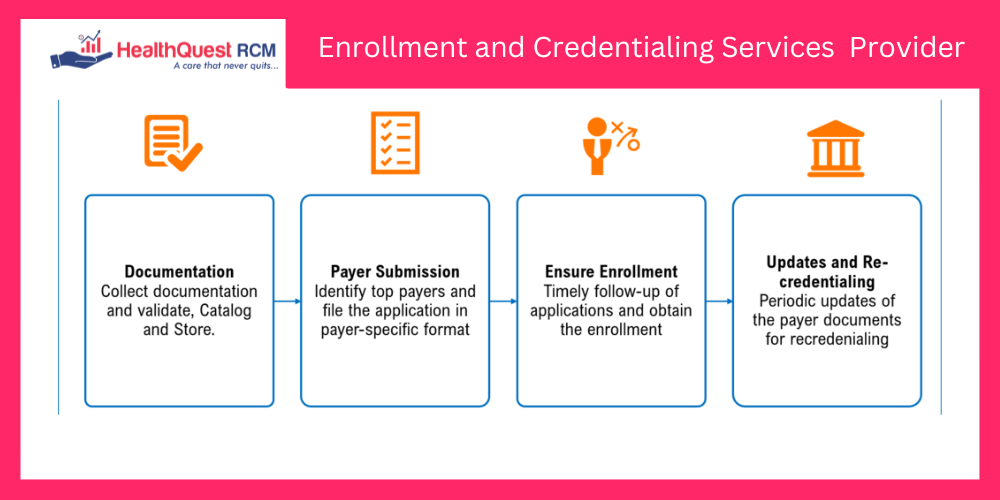
Is there a single point of contact where you can get services for enrollment and credentialing?
- If you have the right service provider on your side, enrollment and credentialing need not be overly difficult.
- Leading revenue cycle management firms offer total end-to-end assistance for the entire process.
- The providers can focus their attention on patient care while the assigned specialists handle the administrative burden thanks to a single point of contact under a reputable vendor.
- Additionally, they provide software programs that allow you to track your deadlines and upload information.
- To maximize the benefits for the providers, the experts also specialize in renewing and upgrading current payer contracts.
Final words
Contact a specialized service to better understand your problems and create a detailed plan for solving them. We further hope that this article has clarified the differences between provider credentialing and provider enrollment.